🌿 Herbal Immunomodulation: How Botanical Compounds Balance Overactive and Underactive Immune Responses

Estimated Read Time: 11–14 minutes
Introduction
The immune system is one of the most intricate regulatory networks in the human body. It protects against infection, repairs damaged tissues, and maintains internal balance. Yet when this system becomes overactive, underactive, or misdirected, it contributes to chronic inflammation, autoimmune disorders, persistent infections, allergies, and long-post-viral symptoms.
Modern immunology confirms that the immune system is not simply “strong” or “weak”—it is dynamic, constantly adapting to stress, diet, infections, microbiome shifts, endocrine signals, mitochondrial health, and environmental exposures.
Herbal medicine offers a category of therapeutics known as immunomodulators—plants that help balance immune activity rather than simply “boosting” or “suppressing” it. These botanicals influence cytokine networks, T-regulatory cells, innate immunity, oxidative stress pathways, and gut–immune signaling in ways now supported by clinical and biochemical research.
This article provides a Mayo Clinic–level, evidence-based review of herbal immunomodulation—explaining how specific botanicals help regulate immune function across chronic illness, post-viral recovery, autoimmunity tendencies, and whole-body inflammation.
1. Understanding Immunomodulation: Balancing, Not Boosting
1.1 The Immune System Is a Regulatory Network, Not an On/Off Switch
The immune system has two major arms:
Innate Immunity
Adaptive Immunity
Dysfunction occurs when either arm becomes:
Immunomodulatory herbs help restore balance, supporting underactive pathways while calming excessive inflammatory signaling.
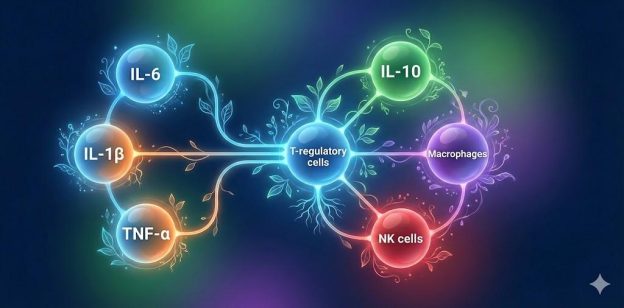
1.2 Cytokines: The Language of Immune Cells
Chronic illness often features disturbed cytokine patterns:
Botanical compounds have been shown to reduce pro-inflammatory cytokines while elevating regulatory cytokines—creating balanced immune communication.
1.3 The Microbiome–Immune Axis
The gut microbiome is one of the most important regulators of immune function.
For a deeper dive, see our article:
🔗 “The Microbiome–Inflammation Axis”
Dysbiosis can cause:
Herbal immunomodulators—such as licorice, fireweed, berberine, pomegranate tannins, and chamomile—often exert their immune effects through microbiome pathways.
1.4 Mitochondria and Immunity
Immune cells require ATP to function.
Mitochondrial dysfunction weakens antiviral and regulatory immune activity.
See our article:
🔗 “The Herbal–Mitochondria Connection”
Herbal compounds that support mitochondrial function indirectly improve immune system resilience.
2. Mechanisms of Herbal Immunomodulation
Herbs influence immunity through several well-described pathways:
2.1 Cytokine Regulation
2.2 T-Regulatory (Treg) Cell Support
Tregs prevent autoimmune overactivity.
2.3 Macrophage and NK Cell Modulation
Important for antiviral defense and tissue repair.
2.4 Antioxidant Defense
Reduces ROS-driven inflammatory activation.
2.5 NF-κB Regulation
For details, see our internal-link article:
🔗 “Botanical Anti-Inflammatory Pathways” (anchor: cytokine and NF-κB modulation)
2.6 Gut Barrier + Microbiome Interaction
Herbs affect mucosal immunity, the first line of defense.
3. Evidence-Based Immunomodulatory Herbs
Below is a detailed clinical review of major immunomodulatory botanicals.
3.1 Astragalus (Astragalus membranaceus)
A classic immune-supportive herb in Traditional Chinese Medicine.
Mechanisms
Clinical Relevance
Astragalus is not used during active autoimmune flare-ups.
3.2 Medicinal Mushrooms (Reishi, Shiitake, Turkey Tail)
Medicinal mushrooms contain beta-glucans—powerful immunomodulatory polysaccharides.
Mechanisms
Clinical Use
3.3 Echinacea (Echinacea purpurea)
Echinacea has dual immunomodulatory activity.
Mechanisms
Clinical Implications
3.4 Elderberry (Sambucus nigra)
Traditionally used for immune support and viral recovery.
Mechanisms
Clinical Relevance
Avoid during acute cytokine storm phases (e.g., uncontrolled severe inflammation).
3.5 Licorice Root (Glycyrrhiza glabra)
Highly relevant for mucosal immunity and adrenal–immune balance.
Mechanisms
Applications
Use DGL form when avoiding glycyrrhizin.
3.6 Andrographis (Andrographis paniculata)
Strong immunomodulatory herb with antiviral relevance.
Mechanisms
Clinical Relevance

3.7 Canadian Immunomodulatory Botanicals
Internal link to the Canadian herbs article
🔗 “Canadian Wild Herbs With Proven Therapeutic Properties”
(anchor: Indigenous immunomodulatory botanicals)
Key examples:
These plants reflect the harsh climates and nutrient profiles of Canadian ecosystems.
4. When Immunity Is Overactive vs Underactive
Immunomodulators work best when individualized.
4.1 Overactive Immunity
Helpful herbs:
Boswellia, turmeric, ginger, green tea, rosemary, medicinal mushrooms.
Linked reading:
🔗 “Botanical Anti-Inflammatory Pathways”
4.2 Underactive Immunity
Helpful herbs:
Astragalus, reishi, andrographis, elderberry, echinacea.
Linked reading:
🔗 “The Microbiome–Inflammation Axis”
4.3 Immune Dysregulation (Overactive + Underactive at the same time)
Seen in:
Consider herbs that rebalance rather than stimulate, such as medicinal mushrooms, rosemary, and ginger.
5. Lifestyle Synergy: Immunomodulators Work Better with Foundations
Botanicals are most effective when combined with:
For further reading:
🔗 “The Herbal–Mitochondria Connection”
6. Safety Considerations
Use with caution in:
General rules
Conclusion
Herbal immunomodulation represents one of the most sophisticated and rapidly expanding areas of integrative medicine. Rather than “boosting” or “suppressing” immune function, immunomodulatory herbs help the body restore balance—reducing excessive inflammation, improving antiviral defense, stabilizing cytokines, and strengthening mucosal and mitochondrial immunity.
When combined with nutrition, lifestyle interventions, and medical oversight, herbs such as astragalus, medicinal mushrooms, licorice root, elderberry, echinacea, and andrographis can support whole-body recovery in chronic illness, post-viral syndromes, and inflammatory conditions.
For a deeper look at related mechanisms, see our companion articles:
These interconnected mechanisms strengthen the foundation of integrative immune regulation.
📚 References