🌿 Botanical Anti-Inflammatory Pathways: How Herbs Influence Cytokines, NF-κB, and the Body’s Inflammatory Switches

Estimated Read Time: 11–13 minutes
Introduction
Inflammation is one of the most complex and fundamental biological processes in human health. It protects against infection, initiates tissue repair, and coordinates immune defense. Yet when inflammation becomes chronic, persistent, or dysregulated, it contributes to a broad spectrum of conditions—including arthritis, asthma, metabolic syndrome, depression, neuroinflammation, irritable bowel disease, autoimmune disorders, and post-viral syndromes such as long COVID.
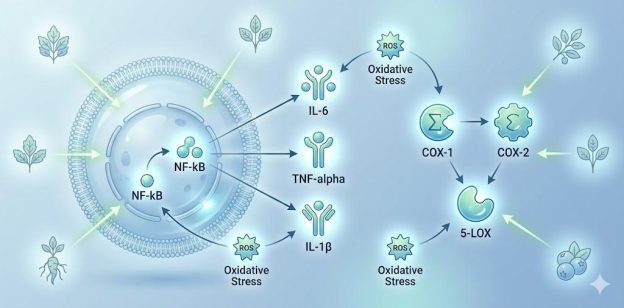
At the molecular level, chronic inflammation is driven by a network of biochemical “switches,” including NF-κB, inflammatory cytokines (IL-6, TNF-α, IL-1β), COX/LOX enzymes, oxidative stress pathways, and the NLRP3 inflammasome. Many of these pathways become activated simultaneously, amplifying the inflammatory burden.
Herbal medicine—when examined through modern biomedical science—interacts with these inflammatory switches in precise ways. Far from being a vague or anecdotal concept, botanical anti-inflammatory activity is now one of the most rapidly advancing fields of phytotherapy research.
This article provides a clinically authoritative, evidence-based review of how specific plant compounds modulate the immune system, influence cytokine expression, regulate NF-κB, and support whole-body recovery from chronic inflammation.
1. Understanding the Body’s Inflammatory Switches
Inflammation is governed by complex biochemical systems. The following are the most clinically relevant pathways targeted by botanical compounds.
1.1 Cytokines: The Immune System’s Communication Network
Cytokines are signaling proteins that coordinate immune responses. Persistent elevation of pro-inflammatory cytokines contributes to:
Key cytokines involved include:
Botanical compounds often demonstrate the ability to reduce pro-inflammatory cytokines and increase anti-inflammatory cytokines (such as IL-10).
1.2 NF-κB: The “Master Regulator” of Inflammation
NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) is one of the most important transcription factors involved in inflammation.
When activated, NF-κB turns on genes responsible for:
Chronic NF-κB activation is implicated in:
Many herbs inhibit NF-κB directly or indirectly—similar to certain pharmaceutical pathways, but generally with multifactorial modulation rather than single-enzyme blockade.
1.3 COX and LOX Enzymes: Pain and Eicosanoid Pathways
The cyclooxygenase (COX-1, COX-2) and lipoxygenase (5-LOX) enzymes convert fatty acids into prostaglandins and leukotrienes—lipid mediators responsible for pain, swelling, and airway inflammation.
While NSAIDs block COX pathways strongly, botanicals tend to modulate, rather than completely inhibit, these enzymes—often with fewer long-term adverse effects.
1.4 Oxidative Stress: The Amplifier of Inflammation
Reactive oxygen species (ROS) damage cell membranes, mitochondria, and DNA. This oxidative stress:
Botanical antioxidants buffer this oxidative load, reducing inflammatory signaling.
2. Evidence-Based Botanicals with Anti-Inflammatory Activity
Below is a clinically rigorous review of the most researched herbs known to influence inflammatory pathways.
2.1 Curcumin (Curcuma longa) — NF-κB, Cytokines, COX/LOX
Curcumin is one of the most extensively studied natural anti-inflammatory compounds.
Mechanisms of Action
Clinical Applications
Curcumin demonstrates multimodal anti-inflammatory effects unmatched by many botanicals.
2.2 Boswellia (Boswellia serrata) — The Primary 5-LOX Modulator
Boswellia resin contains boswellic acids, which strongly inhibit leukotriene synthesis.
Mechanisms of Action
Clinical Evidence
Multiple trials show efficacy in:
Its unique LOX inhibition complements curcumin’s NF-κB suppression.
2.3 Green Tea Catechins (EGCG) — Polyphenol-Mediated Cytokine Regulation
EGCG (epigallocatechin gallate) is a potent antioxidant and immunomodulator.
Mechanisms
Clinical Relevance
EGCG is particularly useful in metabolic inflammation, cardiovascular health, and chronic inflammatory states.

2.4 Ginger (Zingiber officinale) — COX/LOX Dual Modulation
Ginger is among the few botanicals with balanced COX–LOX modulation.
Mechanisms
Applications
2.5 Quercetin — Cytokine and Mast-Cell Stabilization
Quercetin, a flavonol found in apples, onions, and elderflower, exhibits extensive anti-inflammatory activity.
Mechanisms
Clinical Context
Quercetin is relevant to chronic allergic inflammation, viral inflammatory responses, and metabolic inflammation.
2.6 Rosemary (Rosmarinus officinalis) — NF-κB and Complement Modulation
Rosemary contains rosmarinic acid and carnosic acid, two powerful anti-inflammatory polyphenols.
Mechanisms
Applications
2.7 Willow Bark (Salix alba) — Natural COX Modulation
Willow bark contains salicin, a precursor to salicylic acid.
Mechanisms
3. How Herbal Mechanisms Differ from NSAIDs
Feature | NSAIDs | Botanicals |
|---|---|---|
Primary target | COX enzymes | Multi-pathway (NF-κB, cytokines, COX/LOX, oxidative stress) |
Anti-inflammatory reach | Narrow | Broad & systemic |
Effect on gut lining | Irritating | Many herbs support mucosa |
Long-term use | Higher risk | Often safer when clinically supervised |
Immune effects | Suppression | Modulation & balancing |
Herbs do not replace medical treatment but provide nuanced, systems-level modulation appropriate for chronic inflammation.
4. Botanical Synergy: Why Combinations Work Better
Botanicals often work synergistically:
This synergy mirrors traditional herbal formulas used across cultures for centuries.
5. Safety Considerations
Although botanicals are natural, they are pharmacologically active.
Use With Caution:
Avoid if:
Always consult a clinician, especially in chronic disease.
Conclusion
Chronic inflammation is a systems-level disturbance involving cytokines, transcription factors, oxidative stress, and immune dysregulation. Botanical medicine offers scientifically validated tools that modulate these pathways with remarkable sophistication.
Herbs such as curcumin, boswellia, ginger, EGCG, quercetin, and rosemary provide clinically meaningful effects on:
When used responsibly—and integrated with nutritional therapy, sleep, stress reduction, movement, and medical care—these botanicals support whole-body recovery and resilience in a manner consistent with modern integrative medicine.
📚 References